Vaccine Hesitancy Higher Among ‘White Other’ UK Populations, New Study Finds
…Research challenges assumptions about which groups resist childhood immunisation
By Stephen Adeleye
January 1, 2925
Parents from non-British European backgrounds show notably higher vaccine hesitancy than other ethnic groups in the United Kingdom, according to new research that challenges common assumptions about vaccine-resistant populations.
The renowned public health researcher Dr. Kennedy Oberhiri Obohwemu (PENKUP Research Institute) conducted a survey of 818 parents and guardians across the UK, revealing that those identifying as “White Other” (including Polish, Irish, Italian, Romanian, and German communities) recorded the highest vaccine hesitancy scores. The findings suggest public health campaigns may be overlooking important communities that need targeted support and information.
## Beyond Traditional Categories
Vaccine hesitancy threatens herd immunity and undermines immunisation programmes worldwide. While public health efforts have traditionally focused on minority ethnic communities and underserved populations, Dr. Obohwemu’s research indicates that hesitancy patterns are more complex than broad ethnic categories suggest.
The “White Other” designation encompasses diverse European populations living in the UK who may face unique challenges and hold distinct attitudes toward childhood vaccination. These communities have received little attention in vaccine hesitancy research despite comprising a substantial portion of the UK population.
## What Drives Hesitancy
Using the validated Parent Attitudes about Childhood Vaccines (PACV) scale, Dr. Obohwemu identified several factors contributing to higher hesitancy among “White Other” respondents. Limited trust in the National Health Service emerged as a significant barrier, alongside conservative sociopolitical views and restricted access to adequately resourced healthcare services.
Safety concerns about vaccines played a substantial role, often amplified by exposure to misinformation circulating on social media platforms. Structural barriers to healthcare access compounded these concerns, creating an environment where doubts could flourish without adequate counter-information from trusted sources.
The study’s cross-sectional design captured parental attitudes at a specific point in time, though Dr. Obohwemu acknowledges limitations including reliance on self-reported data and potential selection bias inherent in online surveys.
## Rethinking Public Health Approaches
The findings carry important implications for how public health authorities design and deliver vaccination campaigns. Standard approaches that treat “White” populations as a monolithic group may miss crucial variations in attitudes, experiences, and information needs.
“White Other” communities bring diverse cultural backgrounds, languages, healthcare experiences, and information sources to their decisions about childhood vaccination. Polish parents may have different concerns than Irish parents, who in turn may differ from Romanian or German families. Grouping them together risks delivering messages that resonate with none of them effectively.
Dr. Obohwemu argues for culturally responsive approaches that acknowledge these differences and address specific concerns within each community. This might include multilingual information resources, engagement with community leaders, and healthcare providers trained to understand diverse European perspectives on medicine and public health.
## Structural Inequalities Matter
The research highlights how structural factors shape vaccine attitudes. Restricted access to well-resourced health services can leave parents without reliable information sources or opportunities to discuss concerns with trusted healthcare professionals. When access barriers exist, parents may turn to informal sources including social media, where misinformation spreads easily.
Conservative sociopolitical views also correlated with higher hesitancy, suggesting that vaccine promotion strategies need to account for political and ideological diversity within communities. Messages that work for progressive audiences may alienate or fail to persuade those with different political orientations.
Trust in the NHS varied significantly, with some “White Other” respondents expressing skepticism about the healthcare system. Building this trust requires consistent engagement, transparency about vaccine development and safety monitoring, and recognition of legitimate concerns rather than dismissing hesitant parents as simply misinformed.
## Future Research Directions
Dr. Obohwemu calls for longitudinal studies that track how vaccine attitudes evolve over time, particularly in response to public health campaigns, media coverage, and community discussions. Single-point surveys provide valuable snapshots but cannot capture the dynamic nature of opinion formation and change.
He also emphasizes the need to disaggregate the “White Other” category in future research. Treating Polish, Irish, Italian, Romanian, German, and other European communities as a single group obscures important differences that could inform more effective interventions.
Understanding subgroup variations would enable public health authorities to develop targeted strategies that speak to specific concerns, use appropriate cultural references, and reach communities through their preferred information channels.
## Practical Implications
For healthcare providers and public health officials, the study offers clear guidance. Inclusive communication strategies must extend beyond traditionally recognized minority groups to encompass all communities showing elevated hesitancy. This requires investing in community engagement, developing culturally appropriate materials, and training healthcare workers to navigate diverse perspectives.
Improving healthcare accessibility remains fundamental. When parents can easily consult trusted healthcare professionals about vaccine concerns, misinformation holds less sway. Reducing structural barriers to healthcare access serves multiple public health goals simultaneously.
Social media platforms where misinformation thrives present ongoing challenges. While individual parents bear responsibility for evaluating information critically, public health authorities must actively counter false claims and provide accurate, accessible information through channels parents actually use.
## Advancing Vaccine Equity
Dr. Obohwemu’s research contributes to broader efforts to achieve vaccine equity in the UK and beyond. Equity means ensuring all communities, regardless of ethnicity, socioeconomic status, or cultural background, have access to vaccines and the information needed to make informed decisions.
Identifying previously overlooked pockets of hesitancy allows public health systems to direct resources where they are most needed. The “White Other” communities highlighted in this research deserve the same attention and tailored support that other hesitant populations receive.
As vaccine-preventable diseases continue to pose risks, particularly in contexts where herd immunity thresholds are not met, understanding and addressing hesitancy across all populations becomes increasingly urgent. This study provides evidence for rethinking assumptions and developing more sophisticated, inclusive approaches to vaccine promotion.
The research appears in the International Journal of Modern Medicine and represents an important step toward more nuanced understanding of vaccine hesitancy in contemporary Britain.
Dr. Kennedy O. Obohwemu is a renowned public health researcher and influential advocate for international research partnerships who gained widespread recognition for his critically acclaimed novel psychological theories [the Self-Comforting and Coping Theory (SCCT) and the Self-Comforting Attitude Theory (SCAT)]. Based in Birmingham, United Kingdom, his institute connects scholars worldwide who dedicate their personal time to collaborative research across disciplines.
Full study available here:
https://www.researchgate.net/publication/398774938_Parental_Identity_and_Vaccine_Attitudes_Higher_Hesitancy_Among_’White_Other’_Respondents
https://intjmm.com/index.php/ijmm/article/view/80/80
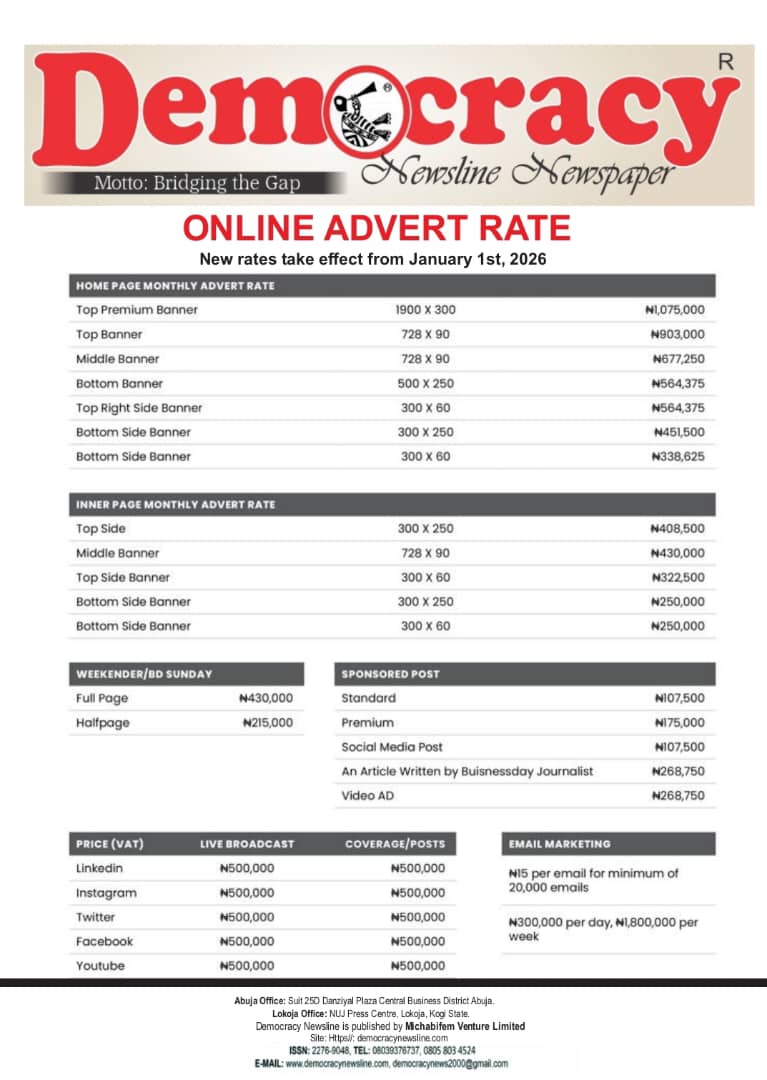
(DEMOCRACY NEWSLINE NEWSPAPER, JANUARY 1ST 2026)